OVERALL CURE RATES
CURE IN 8 WEEKS*
THE ONLY FDA-APPROVED DAA FOR BOTH ACUTE AND CHRONIC HCV1

Acute HCV1,2
100
%
CURE RATE(n=275/275, mITT SVR12)
Single-arm, open-label study of GT 1-4, TN, NC and CC adult participants with acute HCV treated for 8 weeks.
0% on-treatment virologic failure (n=0/286)
0% relapse (n=0/286)
Chronic HCV3
99
%
CURE RATE(n=1218/1226, mITT SVR12)
Integrated, pooled analysis of GT 1-6, TN, NC and CC adult participants with chronic HCV treated for 8 weeks from 8 clinical trials.
0.1% on-treatment virologic failure (n=1/1248)
0.6% relapse (n=7/1226)
Contraindicated in patients with moderate or severe hepatic impairment (Child-Pugh B or C) or those with any history of prior hepatic decompensation.1
*Liver or kidney transplant recipients are not eligible for an 8-week regimen.
mITT population excludes participants who did not achieve SVR12 for reasons other than virologic failure.
Relapse = HCV RNA ≥LLOQ after end-of-treatment response among participants who completed treatment.1
Cure = SVR12 (HCV RNA <LLOQ 12 weeks after the end of treatment)
AASLD and IDSA have not endorsed, and are not sponsors of, or otherwise affiliated with, MAVYRET or AbbVie Inc.
Viral Suppression Across 8 Weeks1,16
In non-cirrhotic patients with chronic HCV completing 8 weeks of MAVYRET
96%
OF PATIENTS WERE VIRALLY SUPPRESSED AT TREATMENT WEEK 4 (n=906/942)
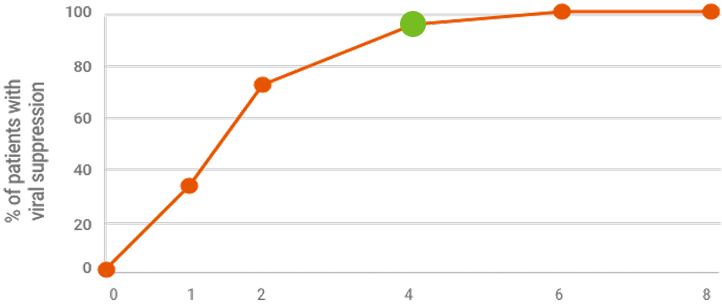
Treatment Week
Viral suppression at treatment week 4 is not a clinical endpoint for cure.
Due to assay difference across studies, LLOQ was 25 IU/mL (Roche COBAS TaqMan® RT-PCR assay v.2.0) or 15 IU/mL (Roche COBAS Ampliprep/TaqMan® RT-PCR assay v.2.0).
METHODOLOGY16
Post hoc exploratory pooled analysis from 5 phase 2/3 clinical trials of chronic HCV GT 1-6, TN or PRS-TE, NC adult patients (N=950) treated with MAVYRET for 8 weeks. HCV RNA was measured at baseline, treatment weeks 1, 2, 4, 5, and at the end of treatment. After excluding patients lost to follow up or missing SVR12 data (n=13) or with on-treatment virologic failure (n=2), 942 had data on viral suppression (defined as HCV RNA <LLOQ).
LIMITATIONS1,16
Product labeling for treatment duration should be followed regardless of HCV RNA levels at treatment week 4. The included clinical studies were not powered to assess the impact of on-treatment viral suppression on SVR12. No conclusions should be made from this exploratory analysis.
96%
OF PATIENTS WERE VIRALLY SUPPRESSED AT TREATMENT WEEK 4 (n=906/942)

Treatment Week
Viral suppression at treatment week 4 is not a clinical endpoint for cure.
Due to assay difference across studies, LLOQ was 25 IU/mL (Roche COBAS TaqMan® RT-PCR assay v. 2.0) or 15 IU/mL (Roche COBAS Ampliprep/TaqMan® RT-PCR assay v. 2.0).
METHODOLOGY16
Post hoc exploratory pooled analysis from 5 phase 2/3 clinical trials of chronic HCV GT 1-6, TN or PRS-TE, NC adult patients (N=950) treated with MAVYRET for 8 weeks. HCV RNA was measured at baseline, treatment weeks 1, 2, 4, 5, and at the end of treatment. After excluding patients lost to follow up or missing SVR12 data (n=13) or with on-treatment virologic failure (n=2), 942 had data on viral suppression (defined as HCV RNA <LLOQ).
LIMITATIONS1,16
Product labeling for treatment duration should be followed regardless of HCV RNA levels at treatment week 4. The included clinical studies were not powered to assess the impact of on-treatment viral suppression on SVR12. No conclusions should be made from this exploratory analysis.
96%
OF PATIENTS WERE VIRALLY SUPPRESSED AT TREATMENT WEEK 4 (n=906/942)

Treatment Week
Viral suppression at treatment week 4 is not a clinical endpoint for cure.
Due to assay difference across studies, LLOQ was 25 IU/mL (Roche COBAS TaqMan® RT-PCR assay v. 2.0) or 15 IU/mL (Roche COBAS Ampliprep/TaqMan® RT-PCR assay v. 2.0).
METHODOLOGY16
Post hoc exploratory pooled analysis from 5 phase 2/3 clinical trials of chronic HCV GT 1-6, TN or PRS-TE, NC adult patients (N=950) treated with MAVYRET for 8 weeks. HCV RNA was measured at baseline, treatment weeks 1, 2, 4, 5, and at the end of treatment. After excluding patients lost to follow up or missing SVR12 data (n=13) or with on-treatment virologic failure (n=2), 942 had data on viral suppression (defined as HCV RNA <LLOQ).
LIMITATIONS1,16
Product labeling for treatment duration should be followed regardless of HCV RNA levels at treatment week 4. The included clinical studies were not powered to assess the impact of on-treatment viral suppression on SVR12. No conclusions should be made from this exploratory analysis.
CURE RATES IN PATIENTS WITH VARIED ADHERENCE17
Based on a retrospective, exploratory analysis of TN, NC or CC patients from 10 phase 3 clinical trials
100%
CURE RATE WITH <90% ADHERENCE
(mITT SVR12)
During weeks 0-4 (n=21/21) and weeks 5-8 (n=76/76)
99%
CURE RATE WITH ≥90% ADHERENCE
(mITT SVR12)
During weeks 0-4 (n=1155/1162) and weeks 5-8 (n=1136/1143)
TELL YOUR PATIENTS THAT IT IS IMPORTANT NOT TO MISS OR SKIP DOSES OF MAVYRET DURING TREATMENT.
METHODOLOGY17
Post hoc, exploratory pooled analysis from 10 phase 3 clinical trials evaluating 8-week treatment with MAVYRET in chronic HCV GT 1-6, TN, NC and CC adult patients. Endpoints include SVR12 and adherence, calculated as the percentage of pills taken relative to the total number expected to be taken during each dispensation interval (weeks 0-4 and weeks 5-8), excluding patients with missing pill count data for that interval.
LIMITATIONS17
The included clinical studies were not powered to assess differences between groups or the impact of adherence on SVR12; therefore, conclusions from this exploratory analysis should be drawn with caution. Patients with stage 4 or 5 chronic kidney disease, or with prior HCV treatment, were excluded. Patients with missing pill-count data were excluded for each interval.
SELECT BASELINE CHARACTERISTICS17
- 9% (n=111/1304) on stable opioid substitution therapy
- 27% (n=349/1304) with history of psychiatric disorder
- 27% (n=351/1304) on ≥5 concomitant medications
- 33% (n=435/1304) currently using alcohol
- 39% (n=510/1304) with history of injection drug use
Patients with a history of psychiatric disorders were self-reported or defined as those with reported concomitant psychiatric medications. Patients using alcohol or with any history of injection drug use were self-reported.
Patient subgroups were not mutually exclusive.
PERCENT OF PATIENTS WITH ≥90% ADHERENCE

TELL YOUR PATIENTS THAT IT IS IMPORTANT NOT TO MISS OR SKIP DOSES OF MAVYRET DURING TREATMENT.
METHODOLOGY17
Post hoc, exploratory pooled analysis from 10 phase 3 clinical trials evaluating 8-week treatment with MAVYRET in chronic HCV GT 1-6, TN, NC and CC adult patients. Endpoints include SVR12 and adherence, calculated as the percentage of pills taken relative to the total number expected to be taken during each dispensation interval [weeks 0-4 and weeks 5-8], excluding patients with missing pill count data for that interval.
SELECT BASELINE CHARACTERISTICS17
- 9% (n=111/1304) on stable opioid substitution therapy
- 27% (n=349/1304) with history of psychiatric disorder
- 27% (n=351/1304) on ≥5 concomitant medications
- 33% (n=435/1304) currently using alcohol
- 39% (n=510/1304) with history of injection drug use
Patients with a history of psychiatric disorders were self-reported or defined as those with reported concomitant psychiatric medications. Patients using alcohol or with any history of injection drug use were self-reported.
Patient subgroups were not mutually exclusive.
